The Mallampati score is a widely used clinical tool for evaluating the potential difficulty of endotracheal intubation. Introduced by Dr. Mallampati in 1983 and later modified by Samsoon and Young in 1985, the scoring system provides a non-invasive, quick, and practical method to assess the visibility of oropharyngeal structures.
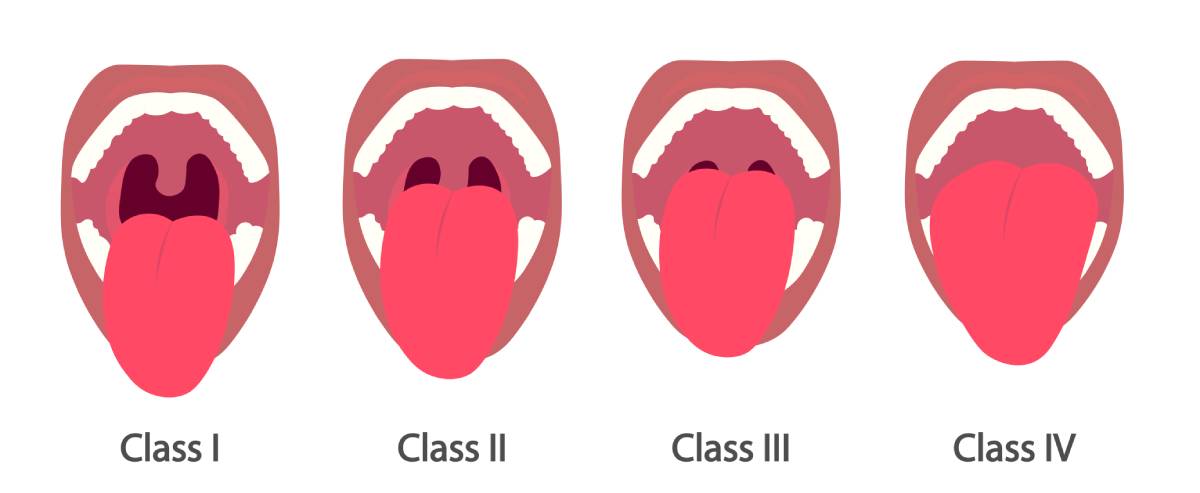
The Mallampati score is determined by having the patient sit upright with their head in a neutral position, open their mouth as wide as possible, and protrude their tongue without phonation. The clinician then examines the oropharyngeal view and classifies it into one of four categories.
Class I reflects full visibility of the soft palate, uvula, fauces, and tonsillar pillars. In contrast, class II reflects visibility of the soft palate, uvula, and fauces, but not the tonsillar pillars. Class III reflects a situation in which only the base of the uvula and soft palate are visible. Finally, class IV reflects a situation in which only the hard palate is visible and the soft palate is not seen. Each higher class correlates with a progressively more challenging intubation scenario, with Class III and IV commonly associated with difficult airways 1,2.
The primary utility of the Mallampati score is in predicting the potential for difficult intubation. Although not a definitive diagnostic tool, it serves as an important component of a broader airway assessment. Studies have shown that higher Mallampati scores are linked to increased incidence of difficult laryngoscopy and intubation. However, the sensitivity and specificity of the test vary across populations and individual assessors, largely due to its subjective nature and dependence on patient cooperation 3–6.
Despite its widespread use, the Mallampati score has limitations. Its inter-observer variability can be substantial, and the classification can differ based on patient positioning, effort, and cooperation. Moreover, the Mallampati score alone is not a perfect predictor of difficult intubation. Its predictive value improves significantly when combined with other airway assessment tools and when anatomical abnormalities or comorbidities like obstructive sleep apnea or obesity are included 7–9.
The Mallampati score remains an essential and accessible element of airway evaluation in clinical practice. While it is not sufficient on its own to predict difficult intubation with high accuracy, it provides valuable initial insight into airway anatomy. When used as part of a comprehensive airway assessment strategy, the Mallampati classification can help guide anesthesiologists and emergency physicians in preparing for potential challenges, thereby enhancing patient safety and procedural success.
References
1. Obstructive Sleep Apnea (OSA): Practice Essentials, Background, Pathophysiology. https://emedicine.medscape.com/article/295807-overview.
2. Stutz, E. W. & Rondeau, B. Mallampati Score. in StatPearls (StatPearls Publishing, Treasure Island (FL), 2025).
3. Kolhe, S. A. & Daokar, S. S. Clinical Assessment of the Correlation Between Tongue Pressure, Modified Mallampati Score, BMI, and Obstructive Sleep Apnea. J Indian Orthod Soc 58, 150–157 (2024). DOI: 10.1177/03015742241221356
4. Dalewski, B. et al. The Usefulness of Modified Mallampati Score and CT Upper Airway Volume Measurements in Diagnosing OSA among Patients with Breathing-Related Sleep Disorders. Applied Sciences 11, 3764 (2021). DOI: 10.3390/app11093764
5. Kanwar, M. S. & Jha, R. S. Importance of Mallampati score as an independent predictor of obstructive sleep apnea. European Respiratory Journal 40, (2014).
6. Harjai, M., Alam, S. & Bhaskar, P. Clinical Relevance of Mallampati Grading in Predicting Difficult Intubation in the Era of Various New Clinical Predictors. Cureus 13, e16396. DOI: 10.7759/cureus.16396
7. de Carvalho, Cl. ístenes C., da Silva, D. M., Leite, M. S. & de Orange, Fl. . via A. Is Mallampati classification a good screening test? A prospective cohort evaluating the predictive values of Mallampati test at different thresholds. Braz J Anesthesiol 72, 736–741 (2021). DOI: 10.1016/j.bjane.2021.09.008
8. Sitot, M., Amare, W. & Aregawi, A. Predictive values of the modified Mallampati test, upper lip bite test, thyromental distance and ratio of height to thyromental distance to predict difficult laryngoscopy in pediatric elective surgical patients 5–12 years old at selected Addis Ababa governmental hospitals, Ethiopia: a multicenter cross-sectional study. BMC Anesthesiology 22, 364 (2022). DOI: 10.1186/s12871-022-01901-4
9. Lundstrøm, L. H. et al. Poor prognostic value of the modified Mallampati score: a meta-analysis involving 177 088 patients. British Journal of Anaesthesia 107, 659–667 (2011). DOI: 10.1093/bja/aer292