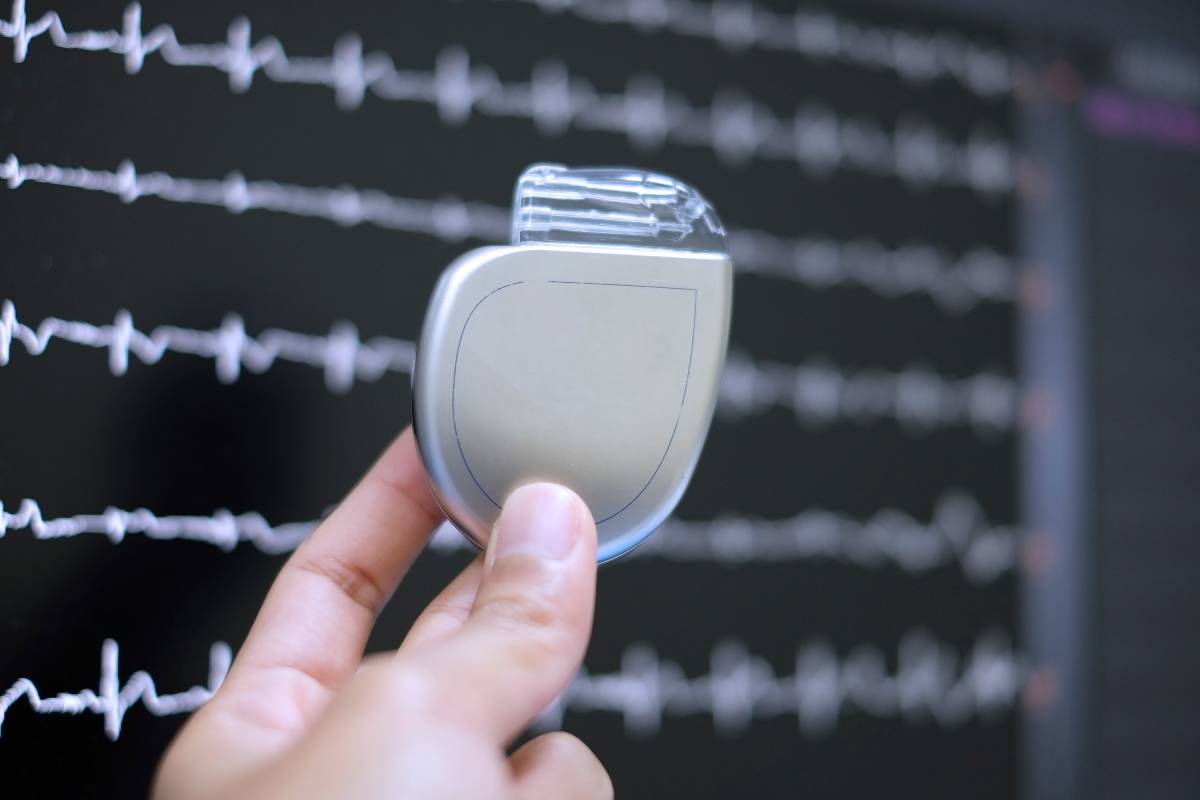
The ubiquity of cardiac implantable electronic devices (CIEDs), such as pacemakers and implantable cardioverter-defibrillators (ICDs), has surged globally. With an increasing number of patients with CIEDs undergoing diverse surgical and interventional procedures, healthcare providers must comprehend the challenges inherent in managing these devices during the perioperative period. This article delineates the critical considerations for preoperative assessment, intraoperative management, and postoperative care, emphasizing the need for a comprehensive and organized approach to guarantee patient safety and device functionality. Device interrogation in the preoperative and postoperative settings, as well as intraoperative monitoring where possible, are ways to reduce the risk of malfunction and unexpected adverse events.
Before embarking on elective procedures involving patients with CIEDs, a thorough preoperative assessment is indispensable. This assessment entails collaboration with the cardiology or institutional CIED care team, the anesthesiologist, and the surgeon. Crucial information to gather includes the type of CIED, manufacturer details, model number, current settings, and the overall functionality of the device. Patients are typically encouraged to carry a manufacturer’s identification card, simplifying the reference process.
The American Society of Anesthesiologists (ASA) recommends CIED interrogation within three to six months before scheduled surgery, ensuring that the device is functioning optimally. The Heart Rhythm Society (HRS) provides more specific timeframes based on the type of device. This step is pivotal in confirming the proper functioning of the device, as subsequent intraoperative management hinges on the accuracy of this information.
The operating room presents a unique set of challenges for patients with CIEDs. Continuous monitoring of cardiac rate and rhythm is imperative, with special precautions for those with CIEDs. Electrosurgery units (ESUs) and other devices generating electromagnetic interference necessitate careful planning to minimize potential malfunctions. While anesthetic agents generally do not impact CIED function, considerations for bradycardia or long QT syndrome may influence anesthetic choices.
The immediate postoperative period demands meticulous attention to patients with CIEDs, including patient monitoring, device interrogation, and possibly device reprogramming. The ASA recommends continuous electrocardiographic and pulse oximetry monitoring, ensuring any deviations are promptly addressed. Reprogramming of CIEDs to their original settings is crucial before the patient leaves a monitored environment, with adjustments made as needed based on the patient’s condition.
Postoperative device interrogation is advised in specific situations:
1. Emergency Surgery: In cases where surgery is performed urgently without the opportunity for preoperative CIED evaluation.
2. Suspicion of Permanent Disabling: If there is suspicion that anti-tachyarrhythmia therapy might have been permanently disabled rather than suspended (e.g., due to magnet use in an older device or outright failure).
3. Inappropriate Shocks or Electromagnetic Interference: Examples include observed delivery of inappropriate shocks or exposure to significant electromagnetic interference (EMI) near the pulse generator.
Professional societies, including the ASA, HRS, Canadian Anesthesiologists’ Society (CAS), and Medicines and Healthcare products Regulatory Agency (MHRA), offer varying recommendations for postoperative CIED interrogation. While some advocate immediate interrogation for hemodynamically unstable patients, others suggest routine monitoring until stability is assured. However, ASA, HRS, and CAS/CCS guidelines align on the importance of postoperative device evaluation. The British MHRA recommends contacting the patient’s CIED clinic for support to confirm device functionality shortly after surgery, without specifying a timeframe.
In conclusion, the escalating prevalence of CIEDs necessitates a comprehensive and organized approach to perioperative care. From meticulous preoperative assessments to thoughtful intraoperative management and vigilant postoperative care, healthcare providers must prioritize patient safety while ensuring optimal CIED functionality. Given the nuanced nature of guidelines from different professional societies, providers should tailor their approach based on individual patient needs, emphasizing a patient-centric approach throughout the perioperative period.
References
1. Pokorney SD, Miller AL, Chen AY, et al. Implantable Cardioverter-Defibrillator Use Among Medicare Patients With Low Ejection Fraction After Acute Myocardial Infarction. JAMA 2015; 313:2433.
2. Rozner MA, Schulman PM. Creating an Anesthesiologist-run Pacemaker and Defibrillator Service: Closing the Perioperative Care Gap for These Patients. Anesthesiology 2015; 123:990.
3. Healey JS, Merchant R, Simpson C, et al. Society position statement : Canadian Cardiovascular Society/Canadian Anesthesiologists’ Society/Canadian Heart Rhythm Society joint position statement on the perioperative management of patients with implanted pacemakers, defibrillators, and neurostimulating devices. Can J Anaesth 2012; 59:394.
4. Schulman PM, Rozner MA, Sera V, Stecker EC. Patients with pacemaker or implantable cardioverter-defibrillator. Med Clin North Am 2013; 97:1051.
5. Powell BD, Asirvatham SJ, Perschbacher DL, et al. Noise, artifact, and oversensing related inappropriate ICD shock evaluation: ALTITUDE noise study. Pacing Clin Electrophysiol 2012; 35:863.
6. Lau W, Corcoran SJ, Mond HG. Pacemaker tachycardia in a minute ventilation rate-adaptive pacemaker induced by electrocardiographic monitoring. Pacing Clin Electrophysiol 2006; 29:438.
7. Gifford J, Larimer K, Thomas C, May P. ICD-ON Registry for Perioperative Management of CIEDs: Most Require No Change. Pacing Clin Electrophysiol 2017; 40:128.
8. Molon G, Perrone C, Maines M, et al. ICD and neuromodulation devices: is peaceful coexistence possible? Pacing Clin Electrophysiol 2011; 34:690.
9. Rooke GA, Lombaard SA, Van Norman GA, et al. Initial Experience of an Anesthesiology-based Service for Perioperative Management of Pacemakers and Implantable Cardioverter Defibrillators. Anesthesiology 2015; 123:1024.